Oregon Health & Science University
PREVENTIVE CARDIOLOGY
Treating Obesity as a Chronic Disease
Cardiology isn’t the first place most patients go for help losing weight. By the time they come to Jonathan Q. Purnell, M.D., an endocrinologist and director of the Center for Preventive Cardiology in the OHSU Knight Cardiovascular Institute, they know obesity puts them at risk for heart disease. They’ve tried diets and exercise plans. But nothing has worked, and they feel defeated and worried.
His first message to them is a powerful one: “It’s not your fault.”
Purnell is among the first preventive cardiology practitioners in the U.S. to treat obesity as a chronic disease, instead of a lifestyle choice. He’s tapping into a new wave of advanced therapeutics to help people lose weight safely and keep it off.
“We have newer, better options for them,” he says. “They will be healthier, they will have fewer heart attacks, they will live longer — and they’ll lose weight.”
OHSU’s Center for Preventive Cardiology brings together experts in cardiology, endocrinology, nutrition and pharmacology to prevent heart disease. It was founded about 10 years ago to put the latest research into practice. While historically preventive cardiology focused on the treatment of lipid conditions, this field is rapidly advancing to incorporate new research showing how the physiology of cholesterol, blood sugar and weight regulation all dovetail together.
Purnell also connects eligible patients with OHSU’s Bariatric Surgery program to consider weight-loss surgery options.
With appropriate medical weight management, patients see their blood pressure, insulin, triglyceride and cholesterol levels drop. Their liver health improves. Less plaque builds up in their arteries. And they can often stop or cut back medications for hypertension, type 2 diabetes, and lipid levels.
“We have newer, better options for them,” he says. “They will be healthier, they will have fewer heart attacks, they will live longer — and they’ll lose weight.”
OHSU’s Center for Preventive Cardiology brings together experts in cardiology, endocrinology, nutrition and pharmacology to prevent heart disease. It was founded about 10 years ago to put the latest research into practice. While historically preventive cardiology focused on the treatment of lipid conditions, this field is rapidly advancing to incorporate new research showing how the physiology of cholesterol, blood sugar and weight regulation all dovetail together.
Purnell also connects eligible patients with OHSU’s Bariatric Surgery program to consider weight-loss surgery options.
With appropriate medical weight management, patients see their blood pressure, insulin, triglyceride and cholesterol levels drop. Their liver health improves. Less plaque builds up in their arteries. And they can often stop or cut back medications for hypertension, type 2 diabetes, and lipid levels.

Dorrian Rhodes, an OHSU bariatrics patient, stays physically active as one way of managing his weight
Why weight loss is difficult
Purnell starts by educating patients about why it’s so hard for them to lose weight.
“They are fighting their physiology,” he says. “They can do their best in terms of lifestyle changes and still come up short.”
Purnell starts by educating patients about why it’s so hard for them to lose weight.
“They are fighting their physiology,” he says. “They can do their best in terms of lifestyle changes and still come up short.”
The reason rests in the hypothalamus, the part of the brain that regulates body weight. The hypothalamus has a set point for weight that it guards closely, within a narrow 10-pound range of what it thinks is normal. It continuously gets hormonal signals about how much we eat and weigh, and adjusts the set point accordingly. The set point is an evolutionary survival tool that goes up on its own but doesn’t go down on its own, Purnell says.
An average person can expect to lose about 4% of their body weight through consistent lifestyle changes alone over the long run. Some people lose more, but that weight will likely come back.
Genetics, hormones, early life stressors, puberty, pregnancy, menopause, medications, and other factors also come into play in determining peak set point, which happens around age 60.
An average person can expect to lose about 4% of their body weight through consistent lifestyle changes alone over the long run. Some people lose more, but that weight will likely come back.
Genetics, hormones, early life stressors, puberty, pregnancy, menopause, medications, and other factors also come into play in determining peak set point, which happens around age 60.
Purnell’s approach to treating obesity took a big step forward in 2021, when the Food and Drug Administration approved GLP-1 receptor agonists, commonly used to treat diabetes, for weight management. These injectable medications mimic hormones that regulate signals of hunger and fullness in the brain, resulting in average weight losses of 15% to 20% and major improvements in blood pressure, diabetes risk, fatty liver, and other cardiovascular risk factors. Previously approved obesity medications typically resulted in 5% to 10% weight loss.
Patients still need to eat healthfully and stay active. But the medications help patients lose weight without counting calories or steps, Purnell says.
Patients still need to eat healthfully and stay active. But the medications help patients lose weight without counting calories or steps, Purnell says.

“We have newer, better options for (patients.) They will be healthier, they will have fewer heart attacks, they will live longer — and they’ll lose weight.”

As director of the Center for Developmental Health in the Knight Cardiovascular Institute and the OHSU Bob and Charlee Moore Institute for Nutrition & Wellness, Kent Thornburg, Ph.D., exemplifies OHSU’s interdisciplinary support for people with obesity.
Eliminating stigma in obesity care
Weight bias creates a significant barrier to treatment, Purnell says. Our society still widely misunderstands obesity as the result of lifestyle choices and doesn’t treat it like other chronic diseases.
Most providers are sympathetic but don’t offer patients much beyond nutrition and exercise advice, apps, books or websites. Providers might not know the importance, safety and effectiveness of the new weight-loss medications. And most insurance plans don’t cover them.
“What we need to do is have more meaningful conversations about medications,” Purnell says. “They should be an option in frontline care.”
OHSU is taking the lead by developing new guidelines for lifestyle, medical and surgical approaches to weight management in primary care. In other efforts:
Purnell’s greatest satisfaction is seeing the response from his patients.
“The first reaction is tremendous relief,” he says. “They have a better understanding of the forces at play and why it’s been so difficult to achieve what society and doctors have been asking of them. They are very, very grateful.”
Weight bias creates a significant barrier to treatment, Purnell says. Our society still widely misunderstands obesity as the result of lifestyle choices and doesn’t treat it like other chronic diseases.
Most providers are sympathetic but don’t offer patients much beyond nutrition and exercise advice, apps, books or websites. Providers might not know the importance, safety and effectiveness of the new weight-loss medications. And most insurance plans don’t cover them.
“What we need to do is have more meaningful conversations about medications,” Purnell says. “They should be an option in frontline care.”
OHSU is taking the lead by developing new guidelines for lifestyle, medical and surgical approaches to weight management in primary care. In other efforts:
- Purnell advocates for policy changes, trains medical students, and gives talks about the importance of obesity treatment in preventive cardiology.
- The preventive cardiology team is working with the OHSU Bob and Charlee Moore Institute for Nutrition and Wellness to support people with obesity in rural communities throughout Oregon.
- OHSU researchers are studying how bariatric surgery and weight loss affect cardiovascular risk. They also participate in clinical trials of advanced therapeutics for weight management.
Purnell’s greatest satisfaction is seeing the response from his patients.
“The first reaction is tremendous relief,” he says. “They have a better understanding of the forces at play and why it’s been so difficult to achieve what society and doctors have been asking of them. They are very, very grateful.”
PREVENTIVE CARDIOLOGY
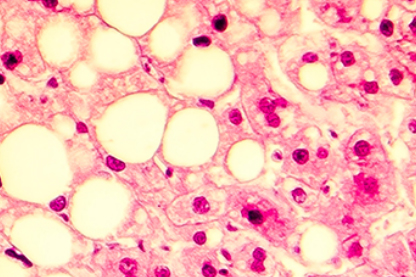
Raising Awareness of Non-alcoholic Fatty Liver Disease
This increasingly common and often undiagnosed condition puts patients at a higher risk for heart attacks.
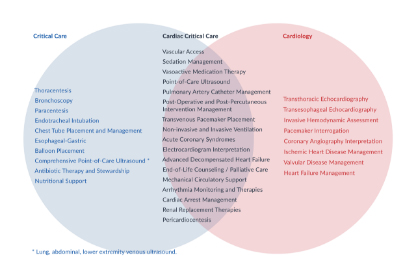
INTENSIVE CARE
Cardiac Critical Care: A Growing Subspecialty
This emerging subspecialty provides a global approach to care for heart patients who have multiple issues.