Oregon Health & Science University
INTENSIVE CARE
Cardiac Critical Care: A Growing Subspecialty
Heart care rarely stops at the heart, especially for the sickest patients. Increasingly, patients in OHSU’s Cardiovascular Intensive Care Unit have complex health issues that involve multiple organ systems and need specialized critical care. That’s where Srini Mukundan, M.D., and Jeffrey Marbach, MBBS, MS, FRCPC, come in.
They are two of the newest cardiologists at the OHSU Knight Cardiovascular Institute (KCVI), and they both have dual training in cardiology and critical care. Together they are establishing OHSU as a national leader in an emerging subspecialty: cardiac critical care.
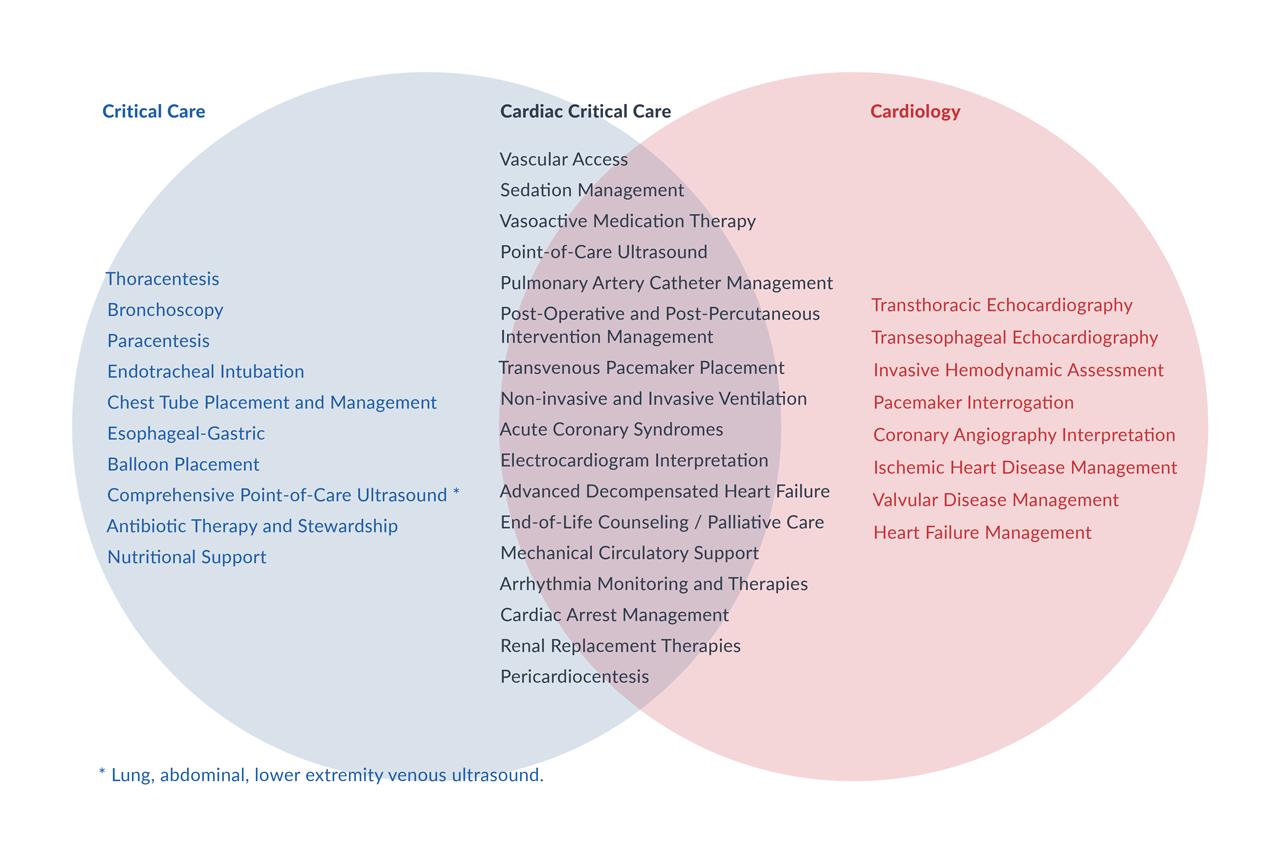
Cardiac critical care, an emerging subspecialty, combines training and experience in cardiology and critical care to support patients with more complex needs.
“Cardiac critical care is an investment into the future of our dynamic and innovative field,” Mukundan says. “I am really excited about the pace at which we are growing.”
More patients than ever are coming to cardiac ICUs with multiple issues, such as sepsis, respiratory failure, and acute kidney injury. Nearly 52% of elderly patients in cardiac ICUs in 2013 had non-heart primary problems, up from 38% in 2003, a national study found. The increase is expected to continue.
More patients than ever are coming to cardiac ICUs with multiple issues, such as sepsis, respiratory failure, and acute kidney injury. Nearly 52% of elderly patients in cardiac ICUs in 2013 had non-heart primary problems, up from 38% in 2003, a national study found. The increase is expected to continue.
Those patients usually need a cardiologist and an intensive care doctor (intensivist). Doctors trained as both can stay with patients longer and manage more of their care, improving relationships and communication.
“Wearing the hat of both the intensivist and the cardiologist requires a global rather than an organ-specific approach to patient care,” Marbach says. “And the result of this is improved communication with patients, and the ability to streamline their care, which is particularly important in times where an acute response and quick decisions are needed.”
Mukundan says dual training has been especially useful during the COVID-19 pandemic, with OHSU’s cardiac ICU opening its doors to an influx of patients with COVID-19. He had the skills to treat acute respiratory distress syndrome, with or without heart complications.
“Wearing the hat of both the intensivist and the cardiologist requires a global rather than an organ-specific approach to patient care,” Marbach says. “And the result of this is improved communication with patients, and the ability to streamline their care, which is particularly important in times where an acute response and quick decisions are needed.”
Mukundan says dual training has been especially useful during the COVID-19 pandemic, with OHSU’s cardiac ICU opening its doors to an influx of patients with COVID-19. He had the skills to treat acute respiratory distress syndrome, with or without heart complications.
He was also ready to care for more patients with ventricular septal ruptures, life-threatening holes in their hearts. Advances in heart care have made these ruptures rare. But during the pandemic, some people having heart attacks delayed going to the hospital for days because they feared getting COVID-19.
By the time Mukundan saw them, poor blood flow had caused ruptures in the heart muscle, resulting in cardiogenic shock. He stabilized patients’ blood pressure, did bedside imaging to better understand how big the ruptures were, and worked with heart surgeons to decide the best timing for repair.
“I was very proud to be part of that team effort,” he says.
By the time Mukundan saw them, poor blood flow had caused ruptures in the heart muscle, resulting in cardiogenic shock. He stabilized patients’ blood pressure, did bedside imaging to better understand how big the ruptures were, and worked with heart surgeons to decide the best timing for repair.
“I was very proud to be part of that team effort,” he says.
Frederick A. Tibayan, M.D., surgery director of OHSU’s advanced heart failure and transplant program, says it is extremely helpful to work with doctors who have dual expertise in heart care and critical care. OHSU’s heart surgery team has extensive experience with complex procedures, including heart transplants.
“We have a shared vocabulary and understanding of what is going on in the physiology of very complicated patients and the management of the ever-expanding array of devices we use,” Tibayan says. “Not infrequently, they make a big difference in a patient’s care and come through in the clutch.”
Training in cardiac critical care is catching up to demand. Doctors complete two fellowships to learn the skills they need. OHSU offers fellowships in cardiovascular disease and critical care medicine, so doctors can do their full training at the academic medical center.
“We have a shared vocabulary and understanding of what is going on in the physiology of very complicated patients and the management of the ever-expanding array of devices we use,” Tibayan says. “Not infrequently, they make a big difference in a patient’s care and come through in the clutch.”
Training in cardiac critical care is catching up to demand. Doctors complete two fellowships to learn the skills they need. OHSU offers fellowships in cardiovascular disease and critical care medicine, so doctors can do their full training at the academic medical center.
OHSU is committed to expanding its cardiac critical care program and fostering the next generation of cardiac intensivists, Mukundan says.
“We are constantly striving to improve our ability to take care of very sick patients, and KCVI is dedicated to being a leader in clinical, educational, and research advancements in cardiac critical care,” he says.
“We are constantly striving to improve our ability to take care of very sick patients, and KCVI is dedicated to being a leader in clinical, educational, and research advancements in cardiac critical care,” he says.

“Cardiac critical care is an investment into the future of our dynamic and innovative field.”

“Wearing the hat of both the intensivist and the cardiologist requires a global rather than an organ-specific approach to patient care.”
CARDIOGENIC SHOCK
Saving More Lives with a Cardiogenic Shock Team
When every minute counts, cardiovascular sub-specialists pull out all the stops to support patients with this life-threatening condition.
CARDIOVASCULAR HEALTH
Joining Forces for Lifelong Heart Care
At the OHSU Knight Cardiovascular Institute, heart care starts before birth and lasts a lifetime in a multi-institutional collaboration.