Oregon Health & Science University
ALZHEIMER’S RESEARCH
Discovery:
Collagen Buildup Leads to White Matter Lesions
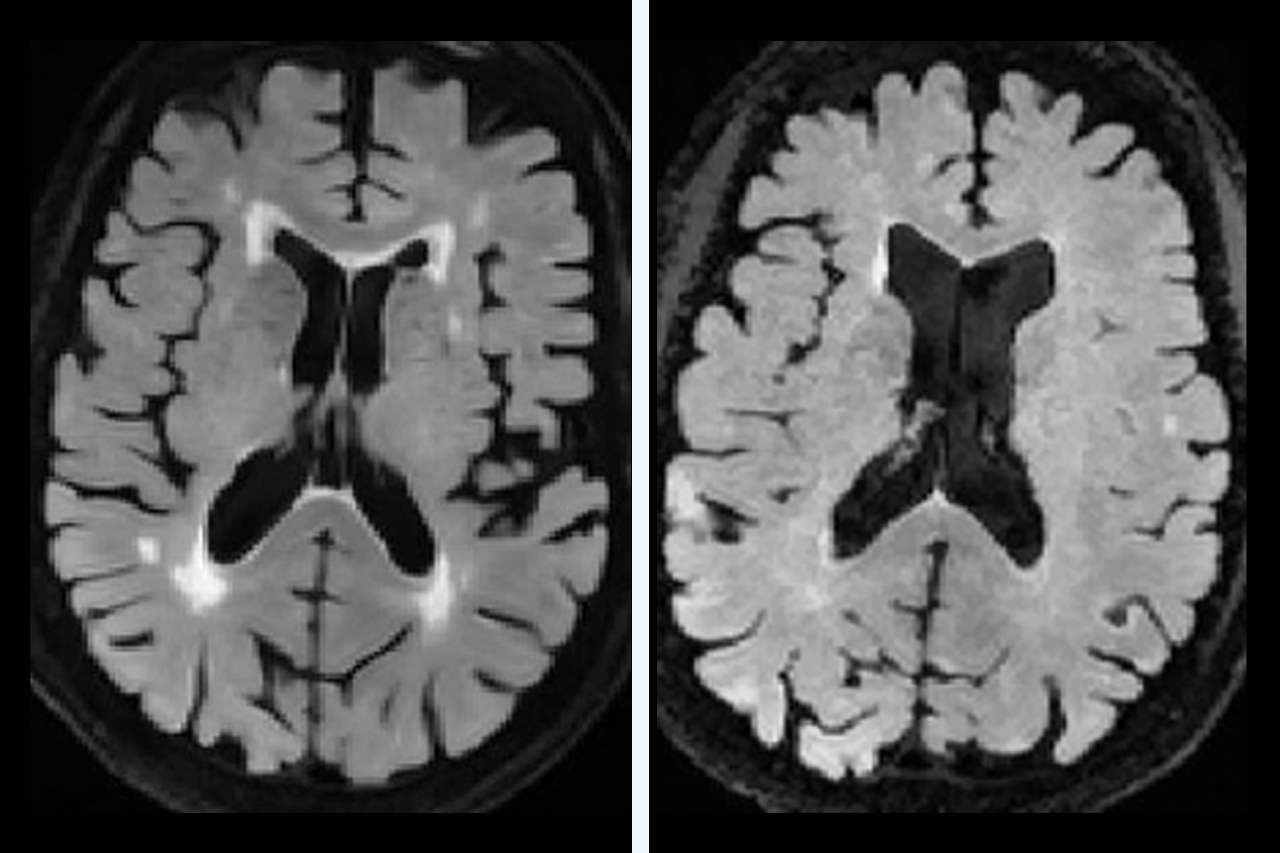
As we age, almost all of us develop changes in our brains’ white matter that show up on imaging as bright spots (white matter hyperintensities). These changes, or lesions, indicate damage to the white matter that is linked to cognitive and motor decline, dementia and stroke.
These images show how OHSU researchers are studying cerebrovascular disease, or conditions that affect blood flow to the brain.
At OHSU’s Layton Oregon Alzheimer’s Disease Research Center, funded by the National Institute on Aging, researchers are helping explain why these brain changes are so common — and what we can do to prevent them.
The researchers led an international study that highlighted an overlooked factor: Buildup of collagen in the veins (venous collagenosis) is a major contributor to age-related changes in white matter around the brain’s ventricles, where age-related damage to white matter is most common.
The researchers led an international study that highlighted an overlooked factor: Buildup of collagen in the veins (venous collagenosis) is a major contributor to age-related changes in white matter around the brain’s ventricles, where age-related damage to white matter is most common.
“It’s this silent brain injury that’s happening to many, many older people,” says Lisa C. Silbert, M.D., M.C.R., who leads the center’s neuroimaging team. “The more we understand it, the more we’re going to find more ways to maintain cognitive health as we get older.”
MRI scans show that up to 97% of older people have some changes or lesions in their white matter, even if they don’t notice any mental or physical changes.
The lesions are signs of damage to the nerve fibers (axons), their coating (myelin), or other changes to cells or small vessels in the brain. The top two risk factors for white matter lesions are increased age and high blood pressure.
The OHSU study suggests that collagen in the veins, likely related to age and high blood pressure-related change, also plays a role.
MRI scans show that up to 97% of older people have some changes or lesions in their white matter, even if they don’t notice any mental or physical changes.
The lesions are signs of damage to the nerve fibers (axons), their coating (myelin), or other changes to cells or small vessels in the brain. The top two risk factors for white matter lesions are increased age and high blood pressure.
The OHSU study suggests that collagen in the veins, likely related to age and high blood pressure-related change, also plays a role.
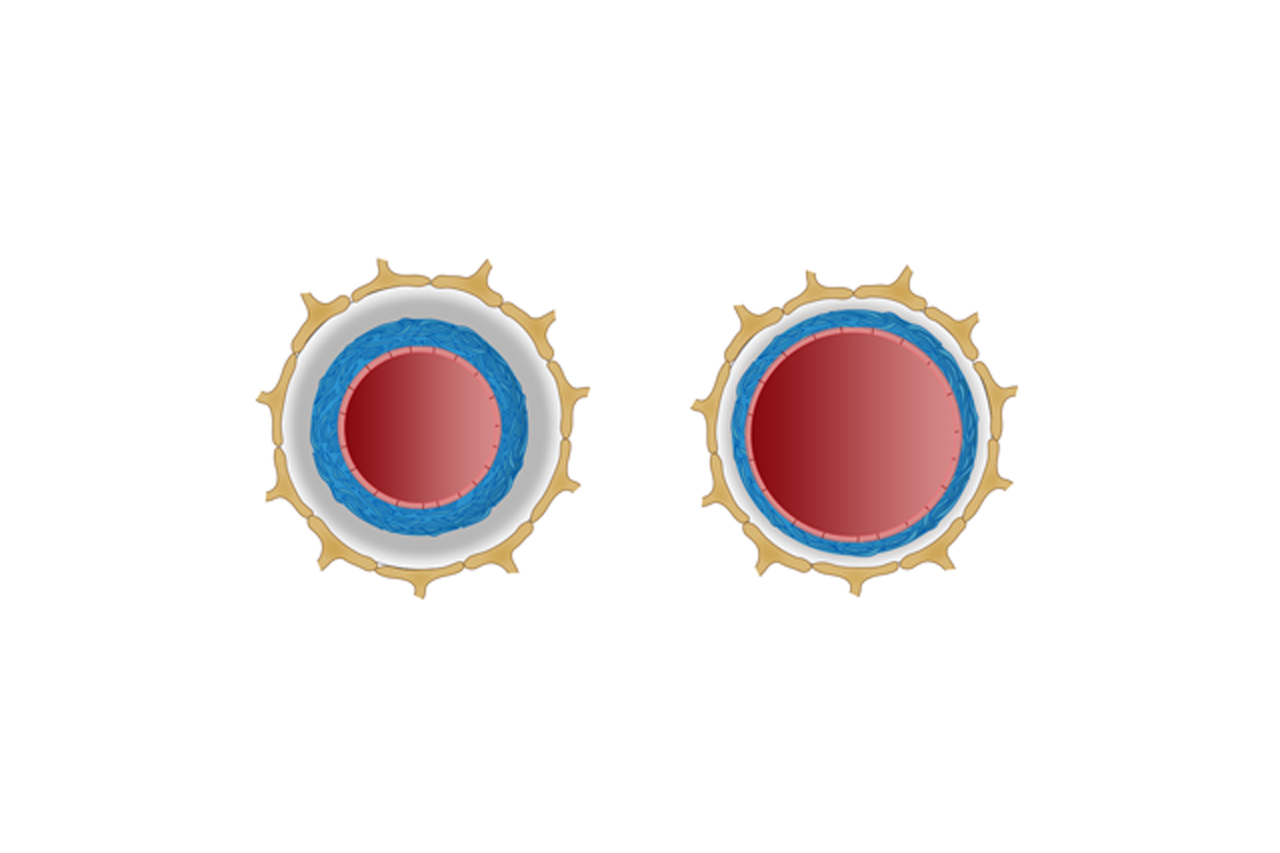
When blood pressure is high, collagen collects on vein walls to protect them from increased stress. The collagen stiffens the vein walls and eventually restricts blood flow and fluid regulation in the brain. Most previous studies have focused on collagen buildup in the brain’s small arteries and have overlooked the veins entirely.
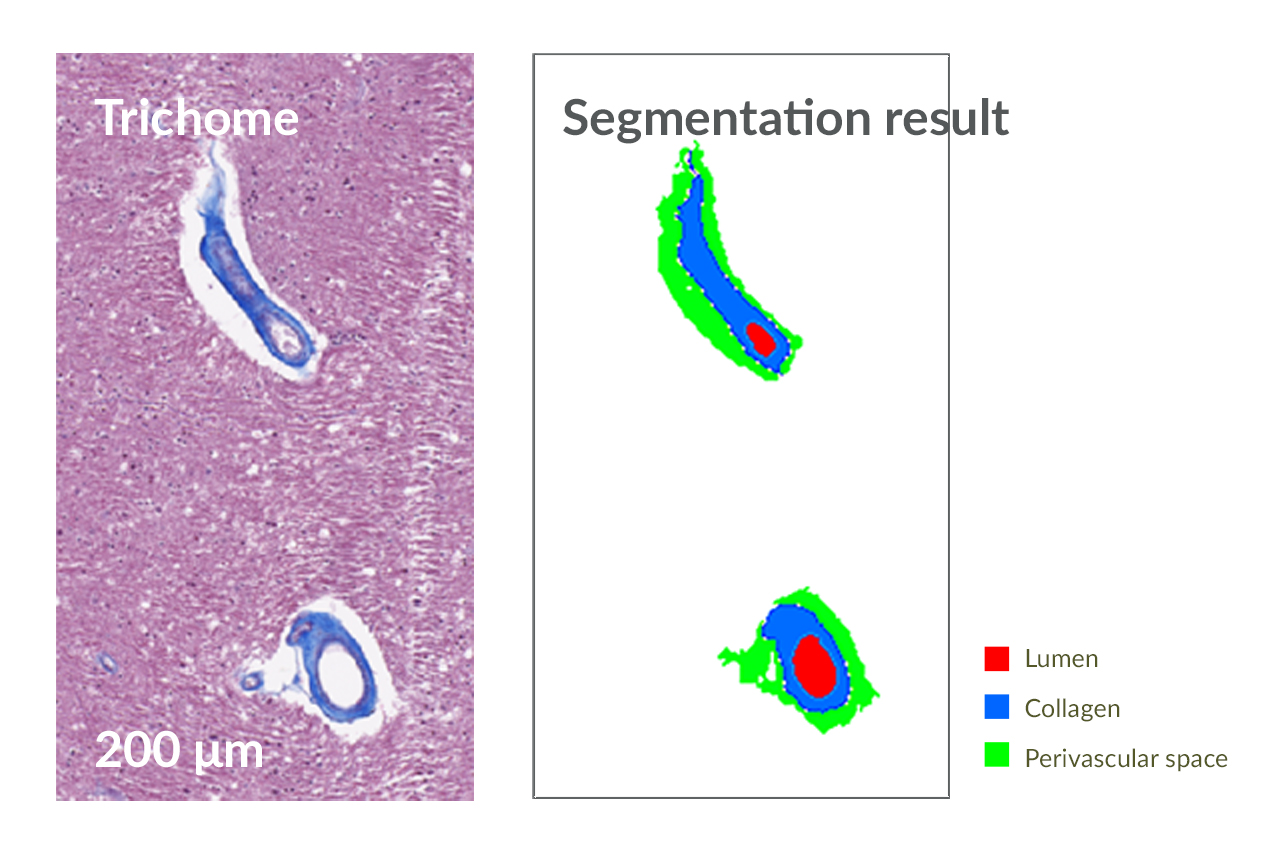
Researchers studied MRI scans and brain tissue of 25 participants in a long-term aging study through the Alzheimer’s research center at OHSU. The researchers used a novel technique comparing MRI images taken during life with digital images of tissue samples donated after death.
Researchers found that collagen thickness in the veins, not arteries, is a significant predictor of white matter lesions around the ventricles. Venous collagenosis likely reduces the body’s ability to clear fluid from between brain cells, resulting in abnormal fluid in the white matter that we see as lesions on MRI.
Silbert says it’s important to focus on modifiable risk factors such as high blood pressure before collagen builds up, ideally in mid-life.
“This is another piece of the puzzle of vascular-related brain injury in older age,” she says. “If we can reverse and prevent it, we’ll have healthier cognitive aging.”
Researchers studied MRI scans and brain tissue of 25 participants in a long-term aging study through the Alzheimer’s research center at OHSU. The researchers used a novel technique comparing MRI images taken during life with digital images of tissue samples donated after death.
Researchers found that collagen thickness in the veins, not arteries, is a significant predictor of white matter lesions around the ventricles. Venous collagenosis likely reduces the body’s ability to clear fluid from between brain cells, resulting in abnormal fluid in the white matter that we see as lesions on MRI.
Silbert says it’s important to focus on modifiable risk factors such as high blood pressure before collagen builds up, ideally in mid-life.
“This is another piece of the puzzle of vascular-related brain injury in older age,” she says. “If we can reverse and prevent it, we’ll have healthier cognitive aging.”

“It’s this silent brain injury that’s happening to many, many older people. The more we understand it, the more we’re going to find more ways to maintain cognitive health as we get older.”
Caring for the Care Partners
Caring for someone with dementia can be stressful and upsetting. A new telehealth program in the OHSU Layton Aging and Alzheimer’s Disease Research Center is making it easier for care partners to receive support and education.

The Tele-STELLA study connects Alzheimer’s care partners with trained guides and with one another for discussions about difficult behaviors and how to address them.
Allison Lindauer, Ph.D., N.P., created the Tele-STELLA study to help care partners manage troubling changes in their family members’ behavior. People with advanced dementia may refuse to shower, make disparaging comments, wander off, have delusions, or become aggressive.
Care partners often feel isolated, Lindauer says. Tele-STELLA offers weekly video sessions to help them connect with one another. They meet one-to-one with a trained guide, then in groups to talk about difficult behaviors and how to address them.
Care partners learn to observe a family member’s behavior in detail and look at what happened before and after. They look for possible reasons for the behavior. For instance, people with dementia might not want to shower because they find the bathroom too cold. Or they might yell because they have trouble finding the right words to express their needs. Armed with this information, care partners can make a plan to improve the behavior.
Care partners learn to observe a family member’s behavior in detail and look at what happened before and after. They look for possible reasons for the behavior. For instance, people with dementia might not want to shower because they find the bathroom too cold. Or they might yell because they have trouble finding the right words to express their needs. Armed with this information, care partners can make a plan to improve the behavior.
 “Giving (care partners) permission to sit back and watch reduces their stress right off the bat.”
“Giving (care partners) permission to sit back and watch reduces their stress right off the bat.”Allison Lindauer, Ph.D., N.P.
Professor of Neurology
OHSU School of Medicine
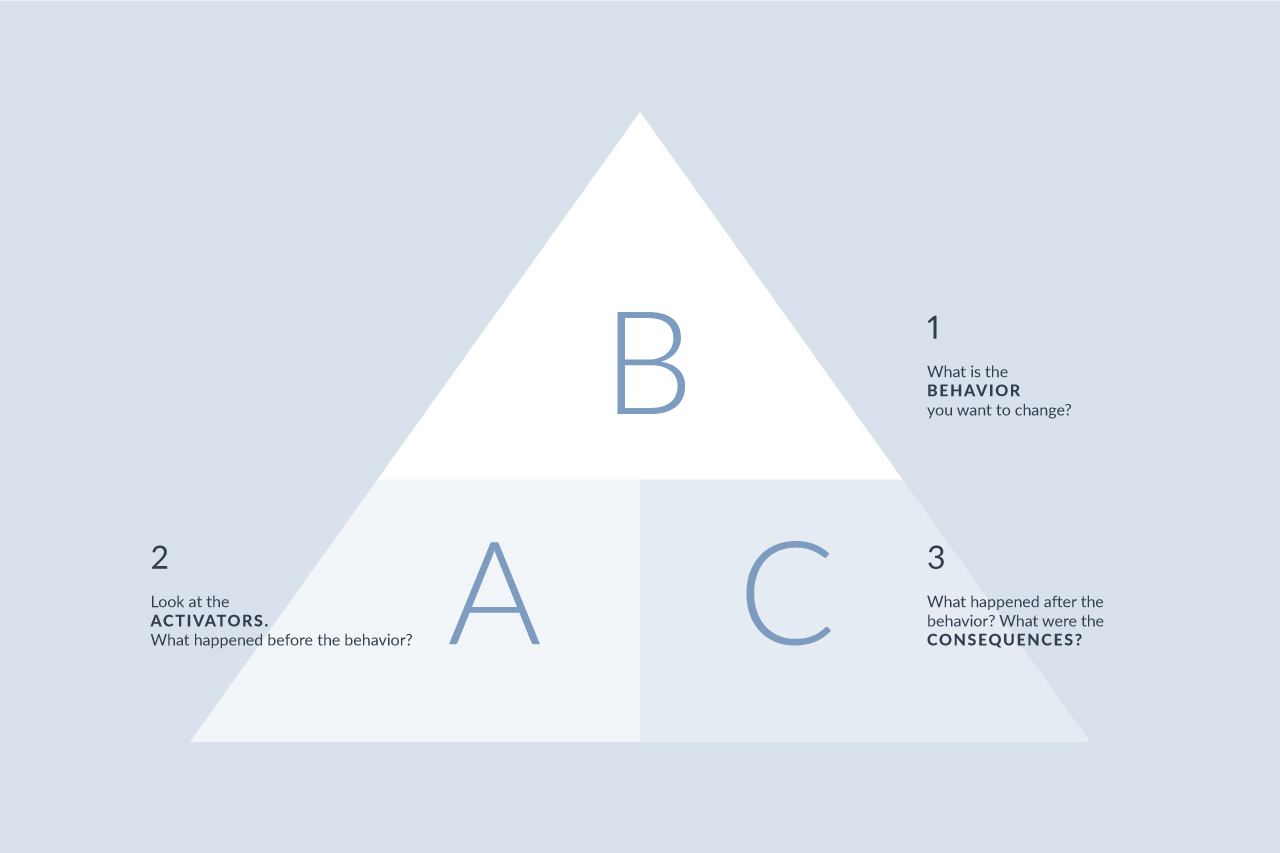
The ABC approach is a tool used in the study to help care partners learn how to identify, manage and change troubling behaviors.
“Giving (care partners) permission to sit back and watch reduces their stress right off the bat,” Lindauer says.
That’s important because care partners often don’t have time or energy to take care of themselves. They are at higher risk of anxiety, high blood pressure and other health issues.
Early results from the Tele-STELLA study are positive. Two years into a five-year study, participants say they like the ease of getting help online from home. They also like meeting other care partners who are on the same path, Lindauer says.
“The reason I love this work is intuitively it makes sense,” she says. “You give people support, and they do better. That’s what we’re seeing.”
That’s important because care partners often don’t have time or energy to take care of themselves. They are at higher risk of anxiety, high blood pressure and other health issues.
Early results from the Tele-STELLA study are positive. Two years into a five-year study, participants say they like the ease of getting help online from home. They also like meeting other care partners who are on the same path, Lindauer says.
“The reason I love this work is intuitively it makes sense,” she says. “You give people support, and they do better. That’s what we’re seeing.”
Give Now
Your generosity supports vital and life-saving programs across OHSU, from groundbreaking cancer research to pediatric care to education.
MULTIPLE SCLEROSIS
Managing MS Symptoms Through Diet
Diet makes a difference for MS patients, but why? An OHSU neurologist aims to find out.
EPILEPSY
At the Forefront of Epilepsy Treatment
Neuroscience physicians and surgeons are helping develop technology and treatments that promise more options and better quality of life for people with epilepsy.